Category: Conditions
Healing Reactions
If the patient has been to more than four physicians, nutrition is probably the medical answer. Abraham Hoffer, MD, PhD Healing Reactions, On the Road to Better Health Summers rich bounty of fresh fruits and vegetables together with its heat, humidity and more leisurely pace invite us each year to lighten up and adopt healthier…
Metabolic Stress
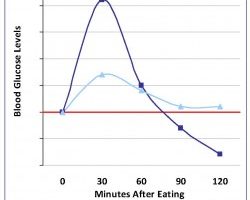
Carbohydrates, in refined form, can lead to blood sugar issues. Yet, traditionallinkcarbohydrateswhole and minimally-processed grains as well as legumes, fruits, and vegetableshelp prevent insulin resistance and chronic disease.link Therefore, to control blood sugar, the answer is not to eliminate carbohydrates. Instead, we need to emphasize traditional carbohydrates, while also using proteins and fats, with their…
Strategies to Avoid Fatty Liver Disease
To read this newsletter in its .pdf form, click here to download the file:June 2011 Newsletter. Thank you. As a sequel to my April and May 2011 newsletters on blood sugar and metabolic stress, this a short June piece on the liver. Spring and summer are the perfect seasons to think of revitalizing the liver….
Dealing with Sugar Cravings
Factors That Underlie Cravings for Sugar For me, a lack of sleep is the biggest force sending me in search of carbohydrates. Besides lack of sleep, stress and emotional upheaval are also big factors that can send us to the cookie jar. Another factor that drives cravings is the relationship of sugar and protein. Carbohydrate…
Managing Inflammation, A Broad Overview
Simple Hows and Scientific Whys Balancing the Inflammatory Response: A Few Simple Steps You Can Take Dietary Ways to Manage Inflammation Lifestyle Approaches to Manage Inflammation Balancing Anti-Inflammatory Omega-3 and Pro-Inflammatory Omega-6 Essential Fatty Acids Refined Flour, Blood Sugar, and Insulin A Segue to ScienceFor a Few Underlying Concepts and Whys Glossary of Terms Summary…

Stress, Cortisol, and Belly Fat
Stress elevates cortisol, and staying up late throws off the bodys natural cortisol rhythm. Because cortisol is the fat storage hormone, chronic stress keeps cortisol elevated and encourages weight gain, particularly in the form of belly fat. The connection between stress and cortisol is one of the reasons that whatever aerobic exercise you choose should…
Diet and Lifestyle that Contribute to Wheat Allergies and Chronic Disease
Wheat allergies and celiac disease, as well as obesity, insulin resistance, diabetes, and chronic disease, are not simply the product of wheat, as Dr. Davis in Wheat Belly might like us to think. Our modern health problems are largely the result of government subsidies that create surpluses of GMO wheat, corn, and soy and the…
Weigh Out: Ideas for Heathy Weight
A persons weight is a product of a variety of factors: hereditary, age, sex, the physical and emotional environment, lifestyle and its associated calorie demands, and the quality and quantity of the food consumed. Gaining or losing weight is far from a linear phenomenon. Some ethnic groups are more efficient at hoarding calories than others,…
Fats and Metabolism
Fats play an important role in weight loss, particularly by making us feel satisfied at the end of a meal. This is intuitive and empirical. And, there are a host of interesting concepts that come from the science lab that support the idea of using healthy, saturated fats for weight loss. Good fats not only…
Thyroid Deficiency and Fertility
Thyroid function and fertility are interrelated. It is estimated that 40% of the population is thyroid deficient. Meanwhile, more women are experiencing fertility issues, particularly as many postpone marriage and childbearing and encounter the stresses of labor force participation. General Diet Guidelines for both thyroid health and fertility coconut oil, cod liver oil, fish oilsthese…