To read this newsletter in its .pdf form, click here to download the file:April 2010 Newsletter. Thank you.
Simple Hows and Scientific Whys
- Balancing the Inflammatory Response: A Few Simple Steps You Can Take
- Dietary Ways to Manage Inflammation
- Lifestyle Approaches to Manage Inflammation
- Balancing Anti-Inflammatory Omega-3 and Pro-Inflammatory Omega-6 Essential Fatty Acids
- Refined Flour, Blood Sugar, and Insulin
- A Segue to ScienceFor a Few Underlying Concepts and Whys
- Glossary of Terms
- Summary Guidelines
- Reading Resources
- Omega-3 Recipes
Read Carols introduction below:
I am not a scientist, of course, but I do like research and sharing information related to nutrition and health. In my work I see inflammation and chronic pain to be issues that disrupt the daily lives and enjoyment of manyand often rather needlessly, it seems. So, in this newsletter I would like to share with you what I have learned over the years from a variety of experts, both in the field of inflammatory disease and in the field of general nutrition and health.
This newsletter aims to outline specific strategies to address pain, inflammation, and chronic disease. But the greater question remains:why is inflammation so pervasive today? Why, in a time of great affluence and food abundance should inflammation and chronic disease be so widespread? The answer lies largely in our modern lifestyle and diet, particularly in the postwar shift away from healthy fats to denatured vegetable oils that foster inflammation while they disrupt the bodys natural metabolism. I will leave this for next months newsletterfor now my focus will be limited to natural ways to control inflammation.
If you are concerned about inflammation, the overarching idea is to try to eliminate inflammatory foodsrefined vegetable oils, trans fats, refined flour, sugar, and high fructose corn syrup. These are not whole foods and they are not in keeping with tradition. They are fractured, empty-calorie foods that fuel the fires of inflammation and chronic disease.
If you take time to read this newsletter, please keep several things in mind. First, that we do need omega-6 oils, but the goal should be to bring these back in better alignment respect to omega-3s, in a ratio of about 3:1 compared to the 20:1 ratio of today:
ourbalance of omega-6 to omega-3 affects our health as much as any other aspect of dietary fatBecause the ratio of omega-6s to omega-3s helps determine the flexibility of cell membranes, nearly all chemical communication throughout the body depends at least in part on the correct balance between omega-6s and omega-3s. Within this context, it is difficult to imagine any health problem that isnt partly related to the ratio of omega-6 to omega-3. link
A second idea to remember is that we need both stable saturated fats like butter and coconut oil for the structural integrity of cell walls, as well as omega-3s and omega-6 fats for the flexibility of cell membranes. Unsaturated omega-3 and omega-6 fats are needed for cells to carry out highly sophisticated neurological and electrical communication functions.
Finally, I mention in this newsletter fish oils and the role that they can play to help cool inflammation, but a supplement like this works best against a supportive diet. The most important step we can take is to shift away from inflammatory foods. By doing so, we remove logs from inflammations burning fire. A fish oil supplement is like placing our trust upon a candle snuffer to put out the flames. Far more important is to stop feeding the fire with inflammatory foods.
Realistically, to eliminate inflammatory foods means that we need to know where our food comes from. This is the very best way to eliminate pro-inflammatory vegetable oils and trans fats that are hidden in prepared foodsas well as inflammatory refined sugars and white flour products.
When we shop for and cook with whole foods that are in keeping with tradition, we naturally incorporate plant foods vital force energy, as well as their antioxidants, phytonutrients, and fiber (July08 newsletter). Plant foods help prevent oxidation and inflammation as they regulate the immune system and assist its proper functioning. Whole foods, sunshine, fresh air, moderate exercise, meaningful life work, and a sense of gratitude are all natural nutrients to build a fertile terrain for our proper genetic expression.
The bodys inflammatory response is vital for survival. It is always on guard and comes to our defense against foreign bacteria, viruses, and other invaders. It also goes to work immediately to help us recover from injury and traumas. Through natural selection, we are genetically prone to inflammation since before the days of antibiotics and modern medicine a strong inflammatory response was necessary in order to survive.
Even though inflammation safeguards our health and wellbeing, in modern times it has acquired a bad reputation. Science tells us to blame inflammation anytime we feel pain, since pain is a sign of inflammation. And, we also know that inflammation, the subtle ongoing silent kind that we do not feel, plays an important role in most, if not all chronic diseaseheart disease, type 2 diabetes, cancer, Alzheimers, arthritis and joint pain, auto-immune disorders, and allergic diseasesto name a few.
If inflammation helped our forebears to survive in a hostile world, why is it now seen as such a health threat? The answer again comes from the science lab. Research tells us that our modern diet and inactive lifestyle are the two factors most to blame for silent inflammation and chronic disease.
In my mind, the diet part of the inflammation story has two sides:
- The shift that has happened in just a few decades away from grass-fed animal products and other foods with healthy omega-3 fats toward processed foods rich in inflammatory omega-6 refined vegetable oils: Today, we consume 25 times more pro-inflammatory refined liquid vegetable oils than a century ago, but only a third as much stable, nutrient-dense butter.
- The transition over the same period away from whole grains and other antioxidant-rich whole foods toward sugars and refined flour products that provide calories but are stripped of vital nutrients. It is really the simple matter of refined productsoils, sugars, and grainsboth crowding out the traditional whole foods that we are genetically programmed to eat, as well as the massive quantities of fractured products in the modern diet that overwhelm the modest levels of good nutrition that we still take in.
Like diet, our lack of exercise also plays a role in the inflammation/chronic disease story. This is because exercise is necessary to moderate insulin, contain abdominal fat,linkand control the bodys naturalinflammatory response. Moderate daily exercise and a healthy diet are two of the most powerful anti-inflammatory strategies of all.
Just think. There is so much that we alone can do to manage and even reverse pain and inflammation without having to rely upon medications. Medications, while sometimes required, work by interfering with the bodys normal processes and their synthetic nature makes them foreign and, to varying degrees, toxic. In contrast, whole foods, with their vital force energy intact, are ideally suited to nourish the human body, cleanse it, and restore it to health.
Because I see inflammation as an underlying factor in many peoples health concerns, I want to use this newsletter to share some thoughts on inflammation. My goal is to keep things simple. Then for those of you who are interested in science, to support these ideas with some underlying concepts related to insulin, belly fat, cortisol, and oxidative stressand the role they play in the inflammatory process (found below).
Balancing the Inflammatory Response: A Few Simple Steps You Can Take
It is true that inflammation is a complex topic, but we do not have to understand it and its underlying dynamics to take actions to overcome its dark side. As mentioned, many scientists have been at work to unravel its mysteries and then guide us in what we should do. Perhaps none is more famous than Dr. Barry Sears. I am indebted to him, as well as to the pioneering work of Mary Enig, Paul Pitchford, Mark Hyman, and a host of others for helping me shape my own thoughts into the following list. While I do not intend to tell you what to eat (we each need different foods), if you are concerned about inflammation, the following measures can be helpful.[Supporting reasons found below.]
Return to the table of contents.
Dietary Ways to Manage Inflammation
- Cut out inflammatory foods. These include processedrefined sugars, grains, and flours; high fructose corn syrup (HFCS); products from grain-fed animals; trans fats; and refined white vegetable oilsespecially those derived from corn, soybean, and cottonseed. These and other cheap, stripped oils are often found in commercial salad dressings and processed foods and are loaded with omega-6 inflammatory fatty acids (Tables 1 and 2, below). Limit consumption of the nightshade vegetablespotatoes, tomatoes, eggplant, peppers, tobaccowhich have an alkaloid, solanine, which can exacerbate pain caused by inflammation.
- Eat whole foods, especially colorful,nutrient-denseplant-based foods rich in anti-oxidant phytonutrients (to contain oxidative stress) and with a low glycemic index (to control insulin). Or, combine higher glycemic color-rich personal favorites with good fats and proteins, which also work to control blood sugar and insulin. [October 07 Newsletter]
- When possible, choose grass-fed animal products, which have an ideal 1:1 ratio of omega-3/ omega-6 fatty acids. This healthy balance of omega-3 and -6 fatty acids means that grass-fed animal products are neutral with respect to inflammation. [September 09 Newsletter]
- Use good fats and oils. For the dinner table choose extra-virgin olive oillow in omega-6 fatty acids, it is essentially neutral concerning inflammation. Also at the table consider flax oil and flax meal [See recipes, below]. For cooking, try stable fats like butter or ghee from grass-fed animals, as well as unrefined coconut oil. Coconut oil is high in lauric acid, an anti-microbial that fights bacteria and viruses that can lead to inflammation.link( Table 2, below)
- Consider a daily fish oil supplement. Fish oil is the most powerful and efficient way to reduce inflammation. Supplementing with fish oil is important because you cannot get enough by eating fish. This is because most beneficial fish oil is in the skin and is lost in cooking; and, of course, the skin is often not eaten. I prefer fermented cod liver oillinkas a rich source of vitamin A, vitamin D, EPA and DHA. EPA inhibits enzymes that foster inflammation, while DHA is vital for brain function. Fish oil is the only direct source of EPA and DHA. For specific tips on using fish oil, see below. [Flax oil is not a comparable substitute for fish oil since it must be converted to EPA. This requires healthy functioning cells and adequate levels of vitamins B3, B6, and C, and magnesium and zincwhich cannot be counted on.]
- Cook with anti-inflammatory herbs, and spices such as turmeric and ginger. These inhibit the enzyme that makes arachidonic acid (AA), the precursor for inflammatory hormones. Turmeric, ginger, and rosemary are also powerful antioxidants.
- Eliminate any potential food allergens (e.g., wheat, corn, soy, egg whites, gluten, dairy, yeast, peanuts) in order to support and restore both intestinal health and immunity (see Probiotics, below).
- Try to buy organic produce, especially when purchasing fruits and vegetables with very high pesticide levels (See Table 3, below). Pesticides and toxins disrupt good intestinal flora and weaken the immune system. Both of these factors create inflammation.
- Consider probiotics (e.g., fermented foods [July 09] or a high-grade probiotic supplement) to maintain and/or to restore good intestinal bacteria. Inflammation is tied to gut health in several ways: First, because good intestinal bacteria are the backbone of the immune system;linkand a healthy immune system is important to manage the inflammatory response. And second, because good bacteria are essential to protect the delicate intestinal wall. The intestine works as a sentryno food enters the blood stream without passing through the mucosal lining of the digestive system. Nothing gets into the body without passing through this barrier. But, this lining is fragile; it is only one cell in depth, and stretched out, spans the size of a tennis court. If the barrier is damaged, toxins and undigested foods can enter the blood stream (leaky-gut syndrome)linkto create allergic reactions and autoimmune disorders.
- Eat adequate protein with each meal to balance blood sugar. The concept of a Barry Sears Zone Diet is to have every meal include moderate portions of protein, carbohydrate, and fat, where a protein serving is defined as 3-4 ounces. This balance curbs insulin (the nutrient/fat storage hormone that responds to blood sugar spikes from carbohydrates) and stimulates the secretion of glucagon (the hormone that assures the flow of glucose for the brain by causing the release of glycogen from the liver).
Return to the table of contents.
Lifestyle Approaches to Manage Inflammation
- Moderate aerobic exercise 5-6 days a week helps prevent insulin resistance. A brisk 45-60 minute walk is perfect. [Excessive exercise, no matter how good the diet, is inflammatory and does more harm than good.link ] Moderate aerobic exercise raises your heart rate and stress level, which forces your cells to become more responsive to taking up glucose from the bloodstream. When this happens, it relieves the pancreas, allowing it to secrete less insulin into the bloodstream. It is important to keep insulin at bay, because insulin boosts arachidonic acid (AA), a precursor of inflammatory hormones.link
- Weight trainingseveral days a weekcan help reduce insulin levels and strengthen immunity. Unlike aerobic exercise which burns fat, strength training burns glucose so it does not directly melt away fat stores. But, by building muscle, what it does do is to make it easier for the body to gobble up glucose from the bloodstream, so less insulin is required. Greater muscle mass also boosts immunity because the body stores amino acids in the muscles, including glutamine, which is a major building block of specialized immune cells.link
- Avoiding visceral (belly) fatcurbs chronic inflammation. This is because the body uses visceral fat as a place to store excess AA (a precursor of inflammatory hormones) in order to prevent high AA levels and inflammation from affecting vital cells. Visceral fat is metabolically active and allows for the steady release of stored AA into the bloodstream, where it can then be taken up by the cells.linkIn short, belly fat fosters inflammation, which leads to more fat deposits, which creates more inflammation.
- A regular relaxation strategy helps lower cortisol levels. Cortisol is an anti-stress hormone whose job it is to turn off the inflammatory response, but constant stress and chronic inflammation keep it elevated. Mediation, yoga, deep breathing or any quiet relaxation for 20-30 minutes a day can help normalize cortisol. And, deep breathing helps to expel toxins, free radicals, and inflammatory agents from the body.
- An early bedtime and enough sleep honors the bodys natural biorhythms. The hours before midnight are the most efficient for restoring the body. Sleep is the bodys own form of natural mediation. Sufficient nighttime sleep allows cortisol to follow its natural cyclical ebb and flow, dropping off around midnight and peaking about sunrise.link
Return to the table of contents.
And now, for a few Whys
Balancing Anti-Inflammatory Omega-3 and Pro-Inflammatory Omega-6 Essential Fatty Acids
If you are a regular reader of this newsletter, you may recall that our forebears consumed a diet that was balanced with respect to omega-6 and omega-3 fatty acids., something around 1:1 or 2:1. But today, for the typical American, this ratio is now is around 20:1, weighted toward inflammatory omega-6 oils. Our modern diet of processed, convenience foods is one factor that explains this shift, since food companies rely upon refined, white vegetable oils like corn, soy, and cottonseed because they are cheap and have a long shelf life (there is nothing left to go rancid). Another aspect is that many modern households have grown to fear healthy saturated fats like butter and unrefined coconut oil and have switched to inexpensive vegetable oils, often believing that they are a healthier choice, and perhaps, too, because they have a long shelf life. Looking at the table below, which outlines the omega-6/omega-3 ratios of a variety of oils, we can easily see how this omega-6/-3 ratio could soar to 20:1. Corn, safflower, and cottonseed oils are frequent ingredients in salad dressings and other prepared foods, and their omega-6/-3 ratios range from 72:1 for corn to 234:1 for cottonseed oil (Table 1, below).
Table 1:Competition of Omega-6s Crowding Out Omega-3s in a Variety of Cooking and Salad Oils
|
Oil
|
Ratio of Omega-6 to Omega-3 (Ideal is 3:1 to 1:1)
|
|---|---|
| Flaxseed | 1/4:1 |
| Butter, Grass-fed animals | 1:1 |
| Walnut | 5:1 |
| Soybean | 7:1 |
| Butter, commercial | 9:1 |
| Olive | 11:1 |
| Sunflower | 19:1 |
| Palm | 46:1 |
| Corn | 72:1 |
| Safflower | 186:1 |
| Cottonseed | 234:1 |
Source: Pathways4Health, Derived from Mary Enigs Know Your Fats
Note: These simply reflect omega-6 versus omega-3s. For a more complete picture and overview, see Table 2 that follows.
Table 2 provides a broader profile of nut and seed oils. It shows omega-3s and -6s fatty acids within the context of other fat components. Note that most oils are a composite of a variety of types of fatty acids. Try to avoid those where the majority of the oil is pro-inflammatory omega-6 such as safflower, sunflower, corn, and soybeanbetween half to three-quarters of these oils are inflammatory omega-6s, with little to no anti-inflammatory omega-3 offset. Olive oil and saturated fats such as butter and coconut oil have very little omega-6s, and are therefore thought to be neutral with respect to inflammation. [Most experts believe saturated fats like butter from grass-fed animals and unrefined coconut oil are good choices unless chronic inflammatory conditions are deeply rooted.link ]
Table 2: Composition of Nut and Seed Oils; A Guide to Choosing Oils to Fight Inflammation
|
Nut or Seed:
|
Super-
Omega-3 (Table) |
Poly-
Omega-6 (Table) |
Mono-
Omega-9 (Low-Temp) |
Saturated
(Cooking) |
Lauric Acid
|
|---|---|---|---|---|---|
| Flax | 58 | 14 | 19 | 9 | 0 |
| Olive | 0 | 8 | 76 | 16 | 0 |
| Coconut,unrefined | 0 | 3 | 6 | 91 | 44 |
| Palm Kernel | 0 | 2 | 13 | 85 | 47 |
| Sesame | 0 | 45 | 42 | 13 | 0 |
| Peanut | 0 | 29 | 47 | 18 | 0 |
| Rape (Canola) | 7 | 30 | 54 | 7 | 0 |
| Almond | 0 | 17 | 78 | 5 | 0 |
| Avocado | 0 | 10 | 70 | 20 | 0 |
| Safflower | 0 | 75 | 13 | 12 | 0 |
| Sunflower | 0 | 65 | 23 | 12 | 0 |
| Corn | 0 | 59 | 24 | 17 | 0 |
| Soybean | 7 | 50 | 26 | 15 | 0 |
| Pumpkin | 7 | 50 | 34 | 9 | 0 |
| Wheat Germ | 5 | 50 | 25 | 18 | 0 |
| Pecan | 0 | 20 | 63 | 7 | 0 |
| Cashew | 0 | 6 | 70 | 18 | 0 |
| Butter (grass-fed) | 1.5 | 2.3 | 29 | 63 | 2.8 |
Source: Udo Eramus and Pathways4Health
Return to the table of contents.
Refined Flour, Blood Sugar, and Insulin
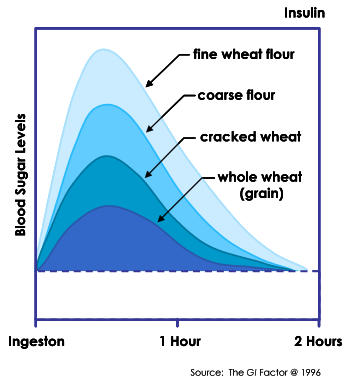 The chart above suggests that whole grains are a better choice than refined flour products for controlling blood sugar. Fracturing a grain raises it blood sugar impact: for example, instant oatmeal (a fractured product) has a glycemic index (GI) of 82 about twice that of steel cut oats (42). If we do choose to eat refined flour products like white bread we can reduce the insulin effect by combining these with low-glycemic proteins/fats (e.g., turkey, eggs, and nut butter). Refined flour is, of course, not eaten alone. It is often baked with ingredients such as eggs, fats, nuts, which lower its GIa sweetened whole-grain muffin can have less impact on blood sugar than a serving of soaked, whole grain brown rice! This may sound strange but I learned this from research on grains and blood sugar by my friend Ellen Arian, a teacher, consultant, and professional whole foods chef.
The chart above suggests that whole grains are a better choice than refined flour products for controlling blood sugar. Fracturing a grain raises it blood sugar impact: for example, instant oatmeal (a fractured product) has a glycemic index (GI) of 82 about twice that of steel cut oats (42). If we do choose to eat refined flour products like white bread we can reduce the insulin effect by combining these with low-glycemic proteins/fats (e.g., turkey, eggs, and nut butter). Refined flour is, of course, not eaten alone. It is often baked with ingredients such as eggs, fats, nuts, which lower its GIa sweetened whole-grain muffin can have less impact on blood sugar than a serving of soaked, whole grain brown rice! This may sound strange but I learned this from research on grains and blood sugar by my friend Ellen Arian, a teacher, consultant, and professional whole foods chef.
Table 3: Produce to Buy Organic to Avoid Pesticide/Herbicides
|
Greatest Load (Buy Organic)
|
Rating
|
Least Load (Buy Regular)
|
Rating
|
|---|---|---|---|
| Peaches | 100 | Onions | 1 |
| Apples | 96 | Avocadoes | 1 |
| Peppers | 86 | Corn, frozen | 2 |
| Celery | 85 | Pineapple | 7 |
| Nectarines | 84 | Mango | 9 |
| Strawberries | 83 | Peas, frozen | 11 |
| Cherries | 75 | Asparagus | 11 |
| Lettuce | 69 | Kiwi | 14 |
| Grapes | 68 | Bananas | 16 |
| Pears | 65 | Cabbage | 17 |
| Spinach | 60 | Broccoli | 18 |
| Potatoes | 58 | Eggplant | 19 |
| Carrots | 57 | Papaya | 21 |
| Green Beans | 55 | Blueberries | 24 |
| Hot Peppers | 53 | Watermelon | 25 |
The Test: The data used to construct the list considered how people normally wash, peel, and prepare the specific produce before eating. The results are compiled from some 42,000 tests for pesticides on produce gathered between 2000 and 2004.
Return to the table of contents.
A Segue to ScienceFor a Few Underlying Concepts and Whys
Insulins Tie to Inflammation: Insulin controls the metabolism and uptake of nutrients by the cellsso it is really a storage hormone, both for fat and for nutrients. A high carbohydrate diet of refined grains/flours and sugars forces the pancreas to speed up insulin production to contain blood sugar levels. Also, with the aging process, people tend to become more resistant to insulin, so the pancreas must produce more insulin to assure that nutrients are taken up by vital cells. When chronically elevated, insulin increases AA levelslink, and AA is a building block of pro-inflammatory hormones. [High insulin levels do not allow the burning of fat since insulin (a storage hormone) prevents the release of fat into the bloodstream. Eating sufficient protein can be helpful for weight loss, both by controlling blood sugar and by stimulating the production of glucagon (See glossary, below).
Abdominal Fats Role in Inflammation: Through natural selection, we are genetically prone to produce large quantities of insulina necessary trait for survival when the efficient storage of calories was critical in times of food scarcity. Now, of course, we live in an environment with readily available refined carbohydrates and sugars and where this traditional fat-storage survival mechanism can easily work against good health, through the accumulation of excess, active fat.
Inflammation and belly fat are closely related because insulin increases AA levels. When this happens, abdominal fat cells are programmed to sequester AA in order to protect vital cells from excessive AA, the precursor of pro-inflammatory hormones. But, when AA accumulates and becomes heavily concentrated in belly fat (the bodys dumping ground for AA), this visceral fat can begin to actively produce pro-inflammatory hormones, which then leads to the production of pro-inflammatory cytokines, which can enter the blood stream and fuel inflammation. As Barry Sears explains: Fat cells can work like immune cells, releasing cytokines as you gain weight. Cytokines make cells resistant to insulin, so the body pumps out more and more insulin, which increases the production of more and more cytokines.link
Cortisols Tie to Inflammation: Cortisol leads to insulin resistance and lowered immune function. Cortisol is the major anti-inflammatory/anti-stress hormone assigned to turn off excess inflammation and the fight-to-flight response. But, under the conditions of chronic inflammation or chronic stresseither emotional or physicalquite the opposite happens. Stress causes cells to produce pro-inflammatory hormonesand, in response, the adrenals pump out more cortisol to try to extinguish the fire. The constant fires that result from chronic stress (stress can stem from excessive exercise, overeating, missing meals, caffeine and other stimulants, excessive weight, etc.) forces the body to counter with more and more cortisol. Thus, chronic stress leads to persistent high cortisol levelsand as your body adapts, you become more cortisol resistant and you need more cortisol. More cortisol leads to more abdominal fat (since high cortisol fosters insulin resistance), as well as a depressed immune system (since cortisols job is to shut off the immune system). Persistently elevated cortisol levels pose a variety of risks, including muscle and bone loss, fat gain, elevated blood sugar, high blood pressure, weakened immune function, loss of memory, and mood swings.link Mediation and other forms of relaxation help to reduce cortisol levels and give the body some breathing time to normalize. A helpful tip when you are unavoidably stressed is to increase your intake of fish oil, as a natural way to help cool and curb inflammation.
Oxidative Stress and Inflammation. Diet is a key underlying factor of oxidative stress and weight gain. A diet centered on sugars and refined carbohydrates and without sufficient antioxidants from whole vegetables and fruits allows free radical damage, known as oxidative stress. Oxidation is a normal process: an apple slice browns when exposed to oxygen, but if dipped in lemon juice, its antioxidants keep an apple slice looking fresh. Oxidation like this also happens inside the body if antioxidants are not sufficient. Oxidation disrupts metabolism, making it less efficient, setting the stage for weight gain. Weight gain and inflammation are, thus, set in motion (see comments about abdominal fat, above).
Plant Foods for Inflammation. Plants are the leading adaptagens. Plants are at the forefront of nutritional innovation, adapting to new environmental conditions and creating the anti-oxidants and phyto-nutrients to survive change. Eating plant foods, especially from our local area, helps us to adapt to the seasons and to longer-term climate shifts. Choosing a wide variety of plant foods across the color spectrum also helps prevent free-radical damage and inflammation. (Table 4, below; and July 08 Newsletter for complete discussion.)
Return to the table of contents.
Glossary of Terms
EPA eicosapentaenoic acid, a prominent ingredient of fish oil, it inhibits the enzyme that converts by-products of omega-6 oils into arachidonic acid (AA), a precursor of inflammation.
DHA dihomo-gamma-linolenic acid, found in fish oil, is vital for normal brain function and can be converted to EPA, so it also plays a role in fighting inflammation.
AA arachidonic acid, is a building block of inflammatory hormones. Excessive dietary levels of omega-6 oils (linoleic acid) relative to EPA and GLA (found in evening primrose oil) fosters AA and inflammation.
ALA alpha-linolenic acidin flaxseed oil, which inhibits the delta-6-desaturase enzymes that decreases both anti-and pro-inflammatory hormones but does little to disarm AA.
Insulinthe nutrient/fat storage hormone that responds to spikes in blood sugar. It has an indirect affect on inflammation by increasing AA levels.
Cortisol an anti-stress, anti-inflammation hormone produced by the adrenals. Its job is to turn off the inflammatory response (the immune system) when it is no longer needed.
Glucagon the major hormone that controls the flow of glucose energy to the brain by signaling the liver to release glycogen.
For a comprehensive scientific explanation of these terms and a thorough discussion of inflammation dynamics, see Barry Sears The Anti-Inflammation Zone.
Return to the table of contents.
Table 4: A Color Spectrum of Fruits and Vegetables
|
Red
|
Dark Green
|
Yellow/Light Green
|
Orange
|
Purple
|
|---|---|---|---|---|
| Apples (Red) | Artichoke | Apples (yellow) | Apricots | Beets |
| Bell Peppers | Asparagus | Apples (Green) | Bell Peppers | Blackberries |
| Cherries | Bell peppers (green) | Avocado | Butternut Squash | Blueberries |
| Cranberries | Broccoli | Banana | Cantaloupe | Cabbage (purple) |
| Grapefruit (pink) | Brussel Sprouts | Bell Peppers (yellow) | Carrots | Cherries |
| Grapes (red) | Chard | Bok choy | Mangoes | Currants |
| Plums (red) | Collard greens | Cabbage | Oranges | Eggplant |
| Radishes (red) | Grapes (green) | Cauliflower | Papaya | Grapes (purple) |
| Raspberries | Green beans | Celery | Pumpkin | Onions (red) |
| Strawberries | Honeydew melons | Fennel | Sweet potato | Pears (red) |
| Tomatoes | Kale | Kiwi | Yams | Plums (purple) |
| Watermelon | Leeks | Lemons | Radish (white) | |
| Lettuce (dark green) | Onions | |||
| Peas | Pears | |||
| Spinach | Pineapple | |||
| Turnip greens | Squash (yellow) | |||
| Zucchini (yellow) |
Source: Textbook of Natural Medicine, J. Pizzorno Jr. and Michael T. Murray
Summary Guidelines
The most important step you can take is to know where your food comes from. This is the best way to avoid excessive pro-inflammatory omega-6 oils and trans fatsand to limit the consumption of refined flours, sugars, and high fructose corn syrup. More specifically:
- Eat good protein (e.g., from grass-fed land animals) with meals to help control blood sugar and insulin;
- Know the good fats and oils. Consider a high-quality fish oil supplement. Use omega-3s and omega-9s (at the table) and saturated fats (for cooking) while you limit pro-inflammatory omega-6s fatty acids.
- Rely on whole grains and fruits and vegetables as carbohydrate sources, rather than sugars and refined flour products, to control blood sugar and insulin as well as oxidative stress.
- Get Moderate Daily Exercise: Do aerobics 5-6 times and strength training 3 times a week, to control insulin and inflammation.
- Get enough sleep to synchronize cortisol and to curb cravings for sugar and refined carbohydrates. The most efficient sleep hours are those before midnight.
- If you take a fish oil supplement, quality matters. Fish oil is best absorbed when taken with other foods. Orange juice or sucking an orange slice helps to dissipate the taste. I believe reliable sources of cod liver oil to be Green Pastures and Radiant Life; and for fish oil, Vital Choice, Omax3, and Pharmax (orange flavored). You may want to research these and others on your own.
If you are concerned about inflammation, ask your doctor for a C-reactive protein (CRP) blood test.
Return to the table of contents.
Reading Resources
- Natasha Campbell-McBride, Gut and Psychology Syndrome
- Mary Enig, Know Your Fats
- Udo Erasmus, Fats that Heal, Fats that Kill
- Mark Hyman, UltraMetabolism
- Bruce McEwen, The End of Stress As We Know It
- Paul Pitchford, Healing with Whole Foods
- Joseph Pizzorno, Jr. and Michael T. Murray, Textbook of Natural Medicine
- Barry Sears, The Anti-Inflammation Zone
- Shawn Talbott, The Cortisol Connection
Return to the table of contents.
Omega-3 Recipeslink
Flax is the richest source of omega-3 fatty acids, but its conversion to EPA and anti-inflammatory prostaglandins requires the presence of vitamins B3, B6, and C, as well as zinc and magnesium. It is useful for the treatment of a variety of issues including inflammatory conditions, cancer, diabetes, high blood pressure and heart disease, immunity, and weight loss (since supports energy metabolism).link
Omega Pesto Sauce
[Omega3: Omega-6 Ratio 1.0 to 0.8 ]
3 cloves garlic
3 T. chopped walnuts
3 T. flaxseed oil
1 T. flax meal
2 T. balsamic vinegar
2 cups fresh basil leaves
cup grated Parmesan cheese
1/3 cup extra-virgin olive oil
In a food processor or blender, add ingredient on at a time, blending after each addition until smooth. Pesto can be stored in an air-tight container in the refrigerator for use within a couple of days.
Can be served as a garnish with fish.
Flax-Olive Oil Vinaigrette
[Omega-3 to -6 ratio 1.0 to 0.4 ]
2 T. flaxseed oil
cup balsamic vinegar
2 T. extra-virgin olive oil
Whisk together. Use on salads and steamed vegetables.
Omega Mixed Green Salad
[Omega-3 to -6 ratio 1.0 to 1.5 ]
8 cups romaine lettuce
2 medium cucumbers
4 cups baby spinach
cup grated carrots
1 cup chopped fresh basil
2 T. chopped walnuts
1 cup chopped fresh parsley
4 T. flax meal
In a large bowl, toss together the romaine, spinach, basil, parsley, cucumbers, and carrots. Scatter walnuts and flax meal over the salad.
Copyright 2010 Pathways4Health.org
Return to the table of contents.
- Haas, Staying Healthy With Nutrition, 68. [link]
- Inflammation and abdominal fat accumulation are inextricably linked, Shawn Talbot,The Cortisol Connection, 35. [link]
- Enig [link]
- Available from Green Pastures and Radiant Life. See January 2010 Shopping Guide. [link]
- See Natasha Campbell-McBride, Gut and Psychology Syndrome, 25-30. [link]
- Primary causes of leaky-gut syndrome include low-fiber, high-sugar, refined-flour, and processed foods; overuse of medications, such as NSAIS, antibiotics, acid blockers, hormones, steroids, and birth control pills; toxins such as mercury and molds; low-grade imbalances, such as yeasts, parasites, and bad bacteria; and stressMark Hyman. [link]
- Dr. Barry Sears,The Anti-Inflammation Zone. [link]
- Sears, 24. [link]
- Sears, 106. [link]
- Sears, 238. [link]
- See Bruce McEwen,The End of Stress as We Know It. [link]
- Art Akers, PhD, Cooling Inflammation; and Mary Enig. [link]
- Sears, 24. [link]
- Sears, 18. [link]
- Talbott, 41. [link]
- Source: Evelyn Tribole, The Ultimate Omega-3 Diet [link]
- Udo Eramus, Fats the Heal, Fats that Kill, 282-3. [link]